Day 3 – Friday 29th April 2005
Jane, Marie, Glenn and I had pretty much been at the hospital since we found out about the accident and all of us were very tired. We could catch the odd 30 minutes sleep in the chairs in the Green Room, but it wasn’t ideal. The hospital were great. They sorted us out a room that we could take turns in using to get some sleep. It was heaven-sent. Marie went first. There was a phone in the room, so if anything went wrong, we could ring her straight away. Jane went next. Unfortunately, Jane has a gammy leg and struggles with long distances and steps. This room was at the furthest point of the hospital (probably about 1/3 a mile away and up 6 flights of stairs). Poor Jane. It was great just to put your head down. We were all out for the count straight away.
In Karen’s first op, they had placed 4 packs in her abdomen area to absorb the blood that was leaking out (of somewhere). They needed to be removed between 24 to 48 hours after placement. So, we were told the plan was for Karen to go back to theatre and to have the packs removed at some point today.
The night wasn’t without its problems………….
“1:50am – Problem with oxygenation. Despite increasing oxygen to 100%, sats only 90%”
Sats are how much oxygen you are able to absorb in your lungs. Normally, it would be about 96% + without being given any oxygen. Karen was being given 100% oxygen and it was 90% – not good.
Marie had a chat this morning with one of the nurses. Here’s how it was recorded…..
“9:00am – Spoken briefly to Karen’s sister Marie and close family. Waiting for review by Catherine with regards plans to remove packs today. If safe to mobilise from bed to trolley. Marie has been expressing concerns regarding resuscitation status and the possibility of organ donation in the event of Karen’s death. Family are aware of high risks involved and minimal chance of survival and wish to discuss “Do not resuscitate” status and potential for organ donation with Catherine in order to make a unified and informed decision. Karen’s husband David is recovering from a recent nervous breakdown and therefore requires adequate support from family, friends and staff during this difficult time.”
It is so hard as I write this now (16 months post accident) to think we were contemplating discussing “Do not resuscitate” Karen. I feel a lot of guilt relating to it. But things were THAT bad. I’ll say no more, or I’ll get upset.
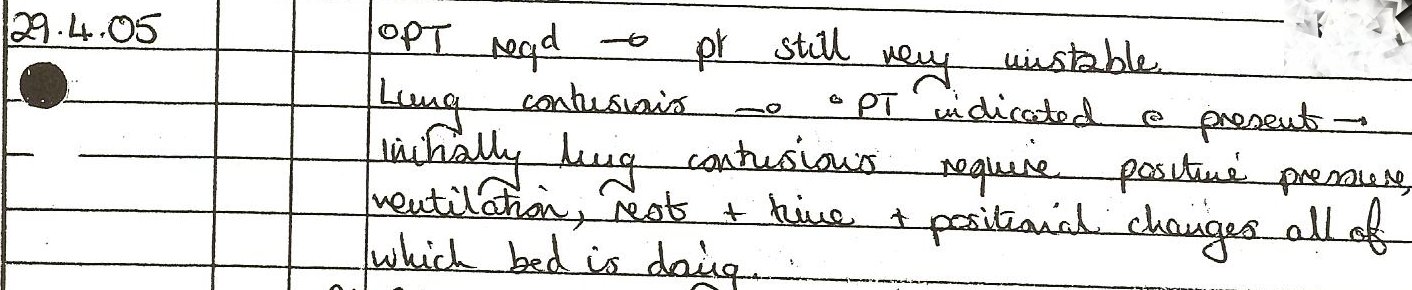
Karen was still very unstable………You’ve heard of the term “Critical, but stable”. There’s only one worse than this and that’s “Critical, but unstable”
Click on photo to enlarge
“1.30pm – Kidney Dialysis Machine clogging up with fat”
This happened time and time again. This machine used these long cylindrical tubes packed with what looked like narrow carbon fibres, through which the blood passed. But the filters continually blocked up with fat, which meant the dialysis stopped and they had to replace the filters at 60 quid a time. They weren’t begrudging the 60 quid, I was just curious. The rotational bed she was in was costing 5000 quid PER WEEK to hire !
Karen was getting oxygen through a mask, and had a tube in her nose (for feeding) and a tube going down her throat so they could keep the lungs clear of fluid. This meant her mouth was constantly open. I recall her tongue looking horrendous – it had lacerations all over it and looked like it had a layer of carpet covering it. The nurses continually were putting Nystatin in it, until we took over and did all the oral care. Her tongue got so bad that in the end, they had to put a trachy tube in so they could remove the tube in her mouth to allow her tongue to heal.
We knew at some point today, they were going to remove the packs from her abdomen. Jane and I were sitting besides her bed. We were a bit stupid for the first few hours. What we’d do is both grab a chair and sit on the side of the bed that Karen was tilting towards. Remember the bed tilted 45′ to the left and then 20 minutes later, it rotated 45′ to the right. So, Jane and I would be holding Karen’s hand and talking to her and then the bed would start it’s slow turn (lasting a minute) to the other side. At which point, something like this would go on…..
Jane :- right Mrs P, your bed’s started to turn, so we’re just going to leave you for a few seconds and go round the other side. We’ll see you when you’re over the other side.
dp:- Yes, won’t be long love. see you round the other side – love you
Jane and I would pick up our chairs, move position and relocate around the other side of the bed.
Jane :- hi Mrs P, welcome back
This would recur every 20 minutes.
And then……………..it dawned on us. Why didn’t one of stay on one side and the other on the other side. So simple, but obviously too much for Jane and I. The nurses must have thought we were stupid !
Anyway, on the afternoon, Jane and I were sitting around one side of her bed and we were watching the cleaning going on around the Intensive Care Unit. We remarked to each other how impressive it was and how thorough they were. There were 2 staff cleaning every surface around the whole ward, even the walls and ceiling !!
We didn’t think anything of it and exchanged positions with Marie and Glenn. When we went back in for our shift, they were finishing up the cleaning. I am sure we made a funny remark about “Do they do homes ?”
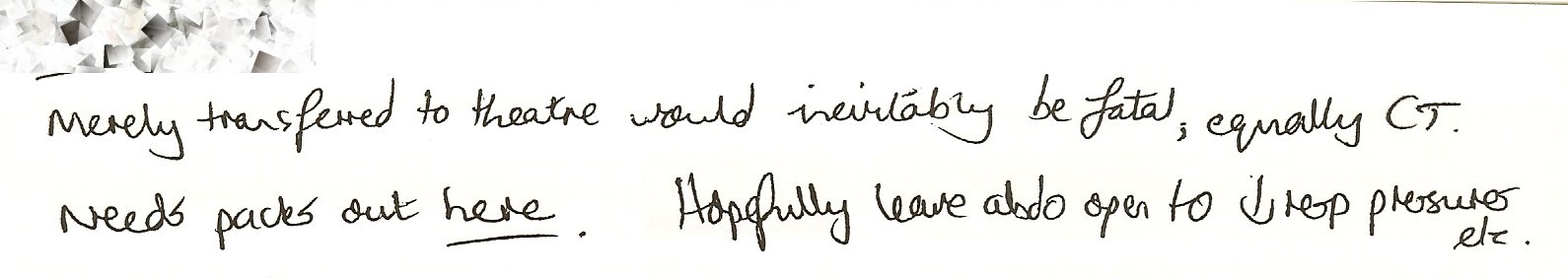
Then, out of nowhere, in waltzed about 7 or 8 operating theatre staff with loads of equipment and they started setting it all up around Karen. We were told that they were going to do the operation to remove the packs in here as it wasn’t safe to move Karen to theatre (it was only 50 m away)
dp:- Should we leave ?
Operating Theatre person :- No, you’re ok for now
And then Jane and I experienced the most surreal experience of our lives. We were sat together in our aprons and gloves in the middle of Intensive Care (about 10 feet from kp) as they built an Operating Theatre around Karen. It was amazing. And we couldn’t believe they were just letting us sit there. It looked like they were about to start operating and we were getting worried that they had forgot about us, but thankfully at that moment, they ushered us out.
Little did we know at the time, how close to death Karen was……………
Click on photo to enlarge
The operation went fine………..
“Abdominal wound opened. Large amount of xx fluid. NO bleeding areas, liver, spleen, bowel looked healthy, all four packs removed. Rectus sheath not closed in otrder to prevent abdominal compartment syndrome.”
The rectus sheath are basically your stomach muscles that keep your insides in. So basically, for the next 15 months, Karen had only her skin between the outside and her internal organs.
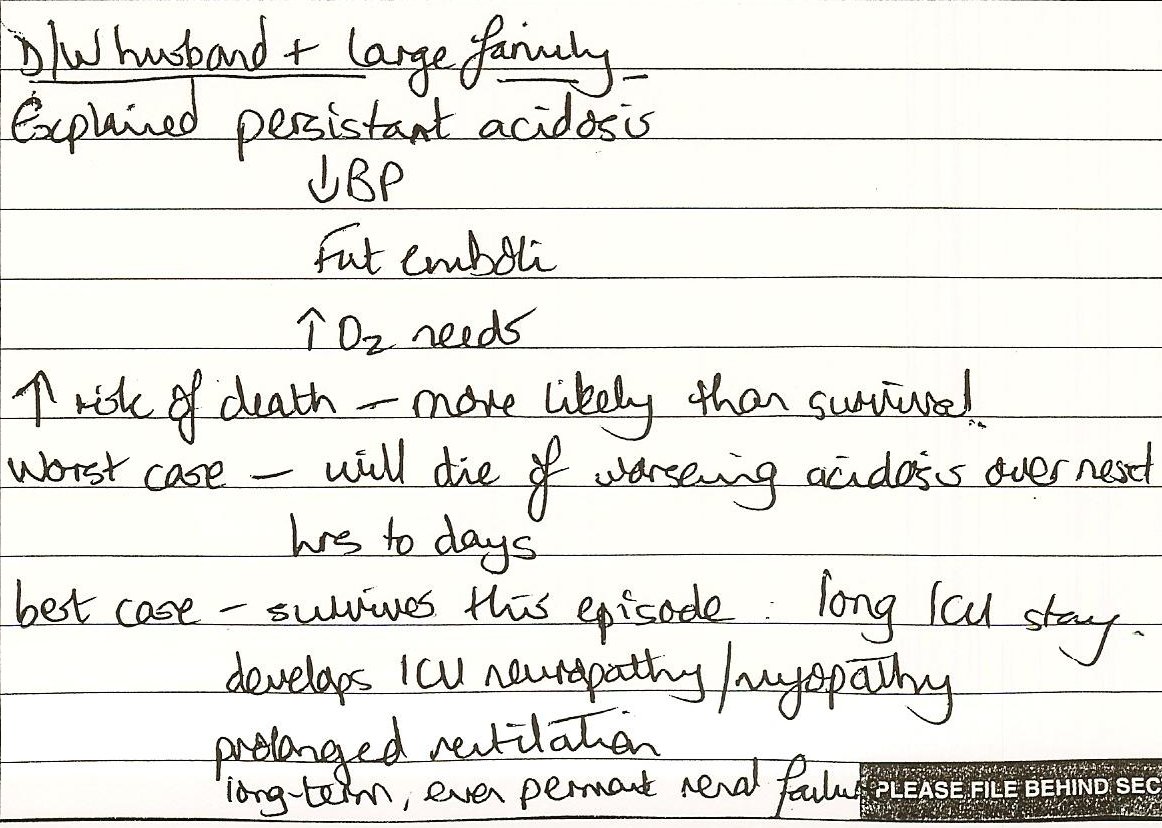
At about 4pm, Catherine (Consultant Anaesthetist) came out to see us in the Green Room……………Here’s how she recorded the converastion….
“Discussed with husband and large family….. 1-Explained persistent acidosis
2-reduced blood pressure
3-fat emboli
4-increased O2 needs.
5-Increased risk of death – more likely than survival.Worst case, will die of worsening acidosis over next hours to days.
Best case…..
1-survives this episode
2-long ICU stay
3-develops ICU neuropathy/myopathy
4-prolonged ventilation
5-long term, even permanent kidney failure
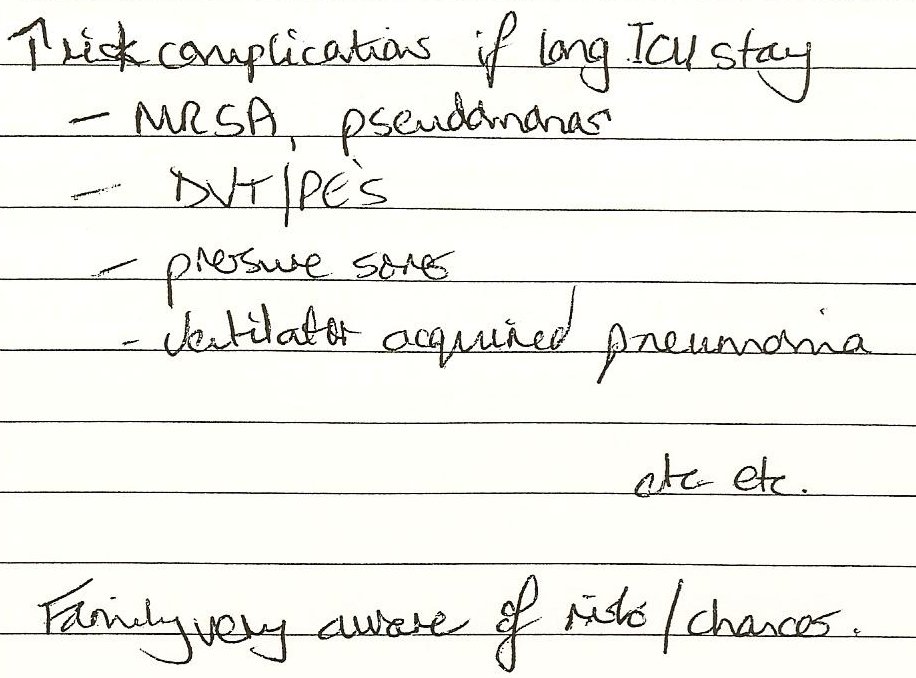
6-Increased risk of complications …….
7-MRSA
8-pseudamonas
9-DVT/PE’s
10-Pressure Sores
11-Ventilator acquired pneumonia etc etc..Family very aware of risk/chances”
Click on photo to enlarge
Click on photo to enlarge
At this, Adele stormed out of the Green Room visibly upset.
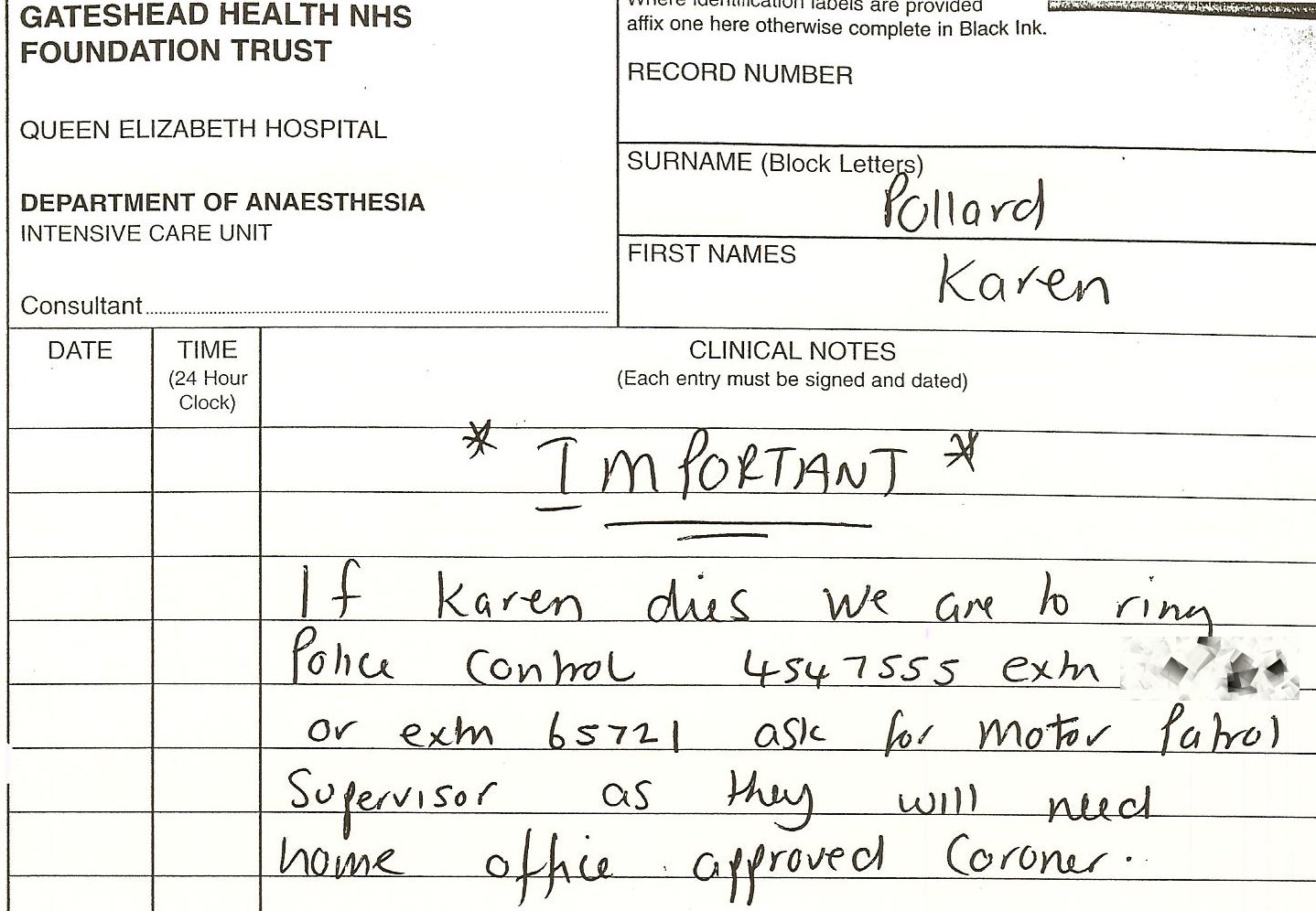
The nurses had left a note in her records saying………….
Click on photo to enlarge