It is hard to put into words our experience as the family and friends of someone critically ill in an Intensive Care ward and someone who we loved very much. The following days and nights lasted an eternity. We cried like babies and laughed like hyenas, experiencing the widest range of human emotion possible.
Karen’s first op was on the Wednesday (27th) evening at 6.35pm. All the family arrived during the operation and we convened in the relatives room, a small room just inside ICU. I had the only one to have seen her before she went in. It was a very anxious wait and the conversation was quite low. To get to the intensive care unit, she would have to be wheeled right past us, so I can remember being very attentive to everyone going past.
At 2245, she was wheeled past us into the Intensive Care Unit (ICU). She was alive. Relief was abundant. Only 2 people could go and sit by her bed in ICU at one time, so Jane and I went in to see her. We had to go through a washing hands, wearing aprons and gloves routine every time we went on to the ward and washing hands on the way out.
I think it’s about week 2 when I started the blog so it’s over 15 months since this day when I write this. I can’t recall how she looked after the first op, but I think she had started to swell up in her hands/face/neck. She was heavily sedated and would be for at least a week. We were told that some people COULD recall conversations that they had heard whilst they were sedated, so Jane and I set about telling her that the operation had been fine and that she would have to “fight” over the next day or so.
Jane :- If anyone can do it, you can do it Mrs P.
We talked for a while and then let Karen’s sisters and other family come in pair by pair.
There was no point us all staying overnight as she had come through the worst (or so we thought), so all the family went home apart from Me, Jane and Marie.
Marie and I went back in again to see her and then Jane and Marie alternated so that I could be there all the time. Whilst Jane was in, Frank (the head anaesthetist honcho and our hero) had stayed on to see her through the night came in to see her whilst we were talking to her. He touched her toes (we thought it a little strange) and then all of a sudden it was action stations. He calmly called people over and then, in his words, further….
“examined karen. Increased Pelvis displacement, increased fluids, discussed with orthopod, recommended to XFix Pelvis.”
She was then ….
“returned to theatre…….unstable……continued blood loss”.

Click on photo to enlarge
This was 2.15am
We phoned all the family who had just arrived home and told them that there had been problems and Karen had been returned to the theatre and it wasn’t looking good. They all set off in another taxi to come back.
Whilst she was in theatre, Catherine came to see us (Frank’s anaesthetist colleague). By this time, the amount of family that had turned up for Karen was too big for us to fit into the small relative’s room inside ICU and we had moved to our new home (The Green Room) just outside ICU. This would be our home for the next few weeks.
Here is how she recorded the conversation to us…..
“Husband and family spoken to by Frank and myself several times overnight to update them on her condition. They are fully aware of her injuries and that they are ON THEIR OWN life threatening. However this does not seemed to have been absorbed so we continue to reinforce that there is a real possibility of death”
Whilst in theatre…..
“4.20am – Clots founds on liver, 4 packs placed in”
“4.30am – Was given 10 Units of Blood and 7 Units of Colloid/Crystalloid”
“5.00am – Returned from theatre. X Fix in place. Good reduction on screening. Increased airway pressures in theatre. OK now, Needs blood and platelets”
“5.15am – Discussed with husband and family. Major setback. Good reduction of fracture but no guarantee that this will stop the bleeding. Given her lots of blood products which means she has an increased risk of lung failure. The pelvic fracture alone now carries a 50% survival rate. No questions asked [by relatives]“
Loss of blood was the key danger to Karen at this time. Her toe being cold had tipped Frank off that she was bleeding internally, hence the rush to theatre.
She was still losing blood at 7.30am…..
“7.30am – Heavy blood-stained urine”
Frank had mentioned, in the night, that they were going to order a special bed for Karen so that she wouldn’t get pressure sores. She was starting to swell up everywhere. Her head ended up being the size of a medicine ball (that sounds like exaggeration, but it’s not), with no neck visible. Her arms and legs were the same, and they were frightened that if she stayed in the same position all the time, her skin would split. This would lead to infection, which would be the last thing she could tackle at the moment. They took Karen’s wedding and engagement ring off at this point as soon they would have to cut them off. I took them and swore to wear them on my little finger until Karen was well enough to have them back. It looked a little (cough) camp, but I didn’t care.
The bed arrived at 8.45am. It was like a medieval torture rack. Karen was placed in it and clamped into position. She was literally clamped in, so that she couldn’t move at all. Her legs were constantly in a v-shape, her arms down by her side, held firm by clamps, her head was also clamped in place by two boards either side. There was no room for any movement, not that she would be doing anyway because of the sedation. Her head was so tightly clamped that she still has scars either side of her head today and probably will for the rest of her life.
Once in this bed, it was switched on, and every 20 minutes, it rotated her from 45′ to the left to 45′ to the right (along the long axis of the bed). Throughout the morning, we spent turns next to Karen’s bedside. She had so many machines all around her. One for monitoring her lungs, one for keeping them going, 2 for her heart, the main vital stats one you see on the tv, 1 for drugs, etc etc……Each of them made strange noises every now and then which got us worried at first, but within a few days, we knew the basics of each machine and had a layman’s understanding of what alarms meant what.
I needed to go home to let the dogs out. Tommy and Eileen (our ace neighbours) had been letting the dogs out last night, but I was going to have to be at the hospital 24/7 for an unknown amount of time, so Jane and I headed home to freshen up and I took the dogs into Kennels so they were no longer a worry. On the way home, Jane and I tried to find Karen’s car so that I could drive it home. Everyone was concerned about me driving, but I was fine. Jane spotted her car at Chester-le-Street and we went home. Poor Dogs didn’t have a clue where their mum was. Feeling refreshed we headed back to the hospital.
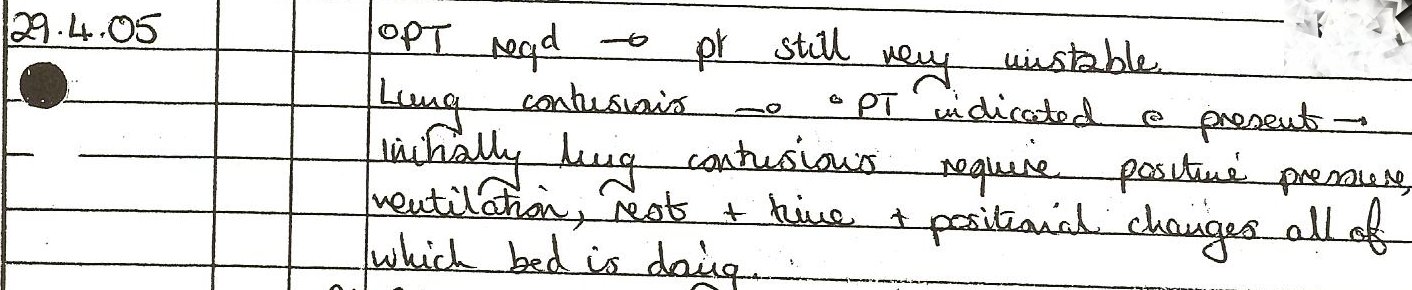
The consultant’s notes carry on reading grim………I don’t know what some of this means, but the last part sounds bad either way….
“1.20pm – Frank discussed (D/W) with [another consultant]…..traumatic SIRS”

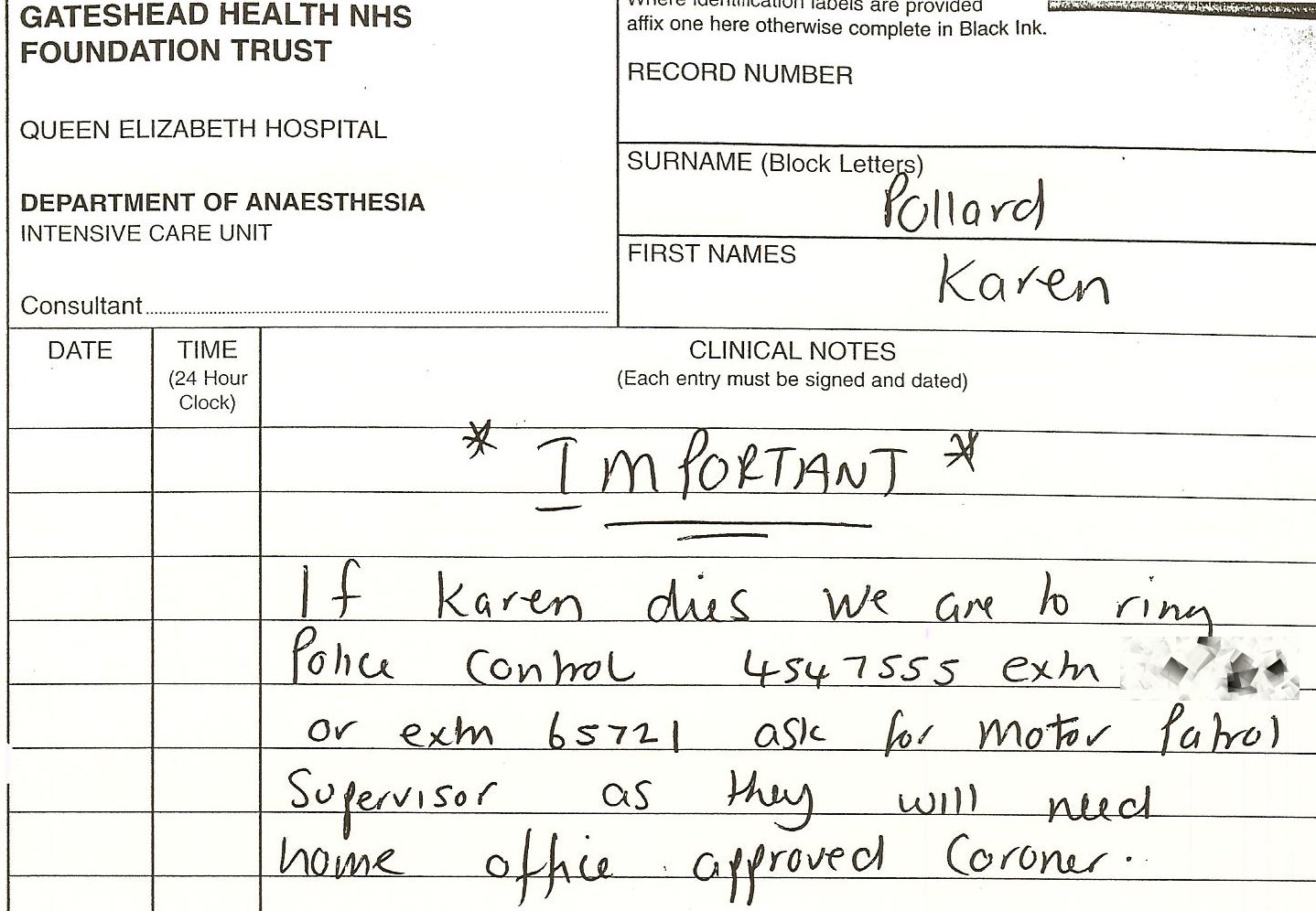
Click on photo to enlarge
SIRS is Septic Inflammatory Response Syndrome and it is a precursor to MOF (Multiple Organ Failure) which is a precursor to D (Death). You’ve got to laugh when you read all these notes. They abbreviate everything. Death isn’t actually “D” – it’s the sign of the cross. At least you can read it, I suppose.
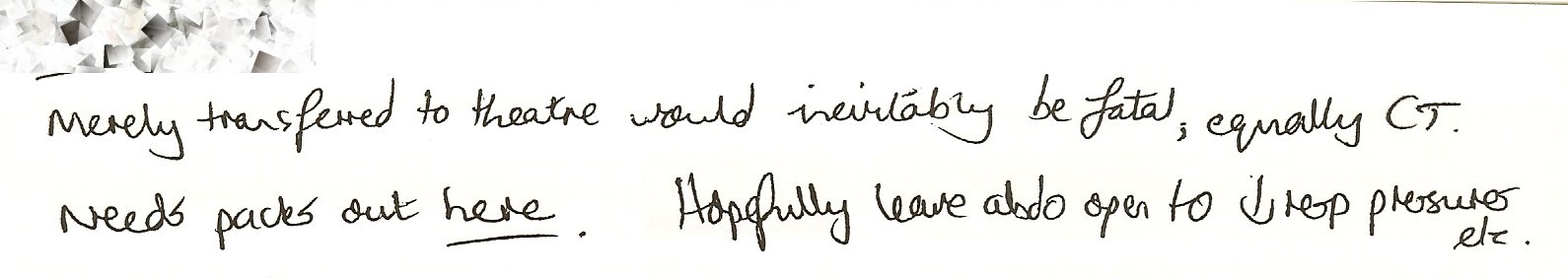
“1.20pm – Current Scenario – Increased Fat Emboli, recommend treat with prostacyclin especially if acid base worsens = this will result in ARF (Acute Renal/Kidney Failure) – probable ANYWAY.”

Click on photo to enlarge
One of the problem with broken bones, especially the pelvis and leg bones (because of their size) is that the marrow can escape into the blood stream (they call it Fat Emboli) and the danger is that they can travel to the brain, heart or lungs and cause death. So this was a big worry for a few days. Aware of this, they put her on blood thinning drugs, but this was the big balancing act. Too thin and she was going to rebleed, which would be fatal, not thin enough and the Fat Emboli could bung up the brain, lungs or heart, causing death … very much the old “rock and a hard place” scenario.
At 2pm, Frank came to see Jane and I ……………..
“Husband David and friend Jane spoken to by Frank re Karen’s further deterioration this afternoon. Explained about possible failing kidney and probable need for filtration which itself carries great risk re further poss of bleeding. Explained that the right side of karen’s heart is struggling due to high pulmonary circulatory pressure”
At 2.20pm, things were still looking dire……..
“Urine still blood stained”
The afternoon dragged on……………things were getting worse…………..
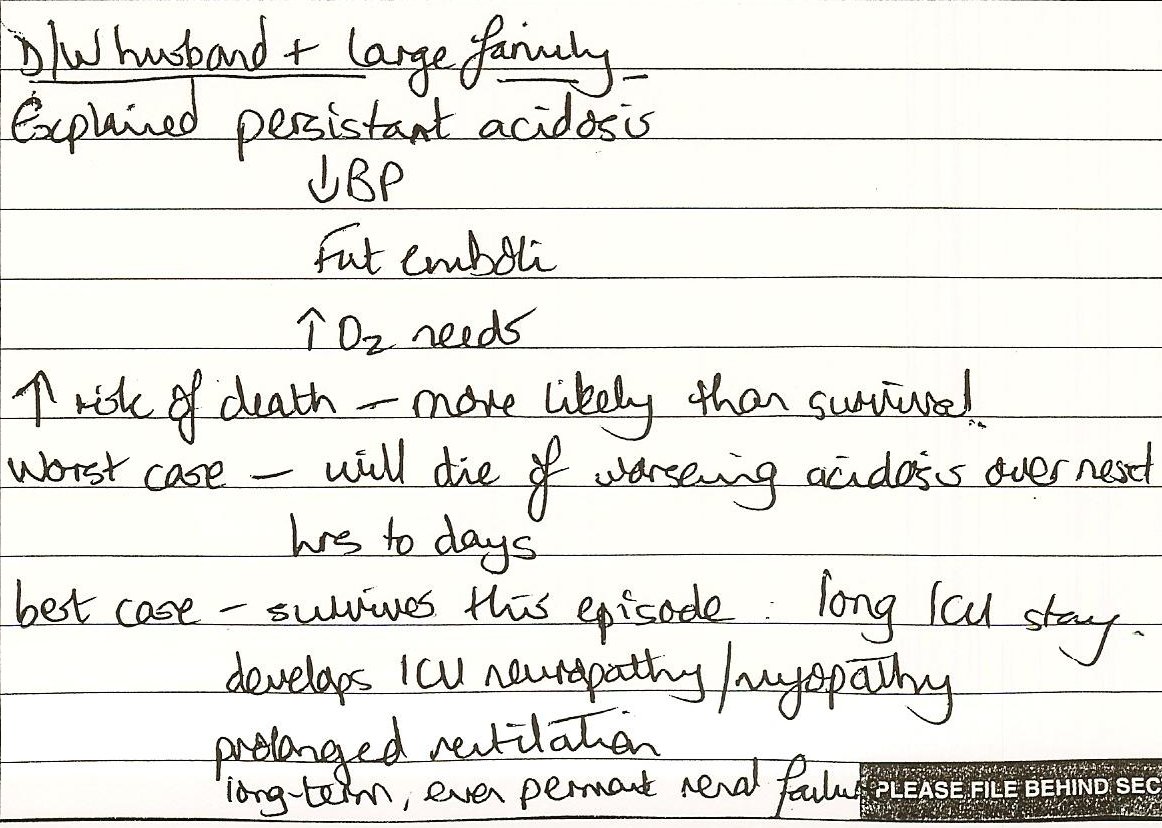
“4.30pm
Discussed with husband, increasingly life threatening condition.
1 – Increased abdomen pressure
2 – fat into lungs (increased back pressure), being put on nebulizer and viagra
3- Kidneys failing, risk of bleed
Asked risk of death, advise risk of death > 75%”

Click on photo to enlarge
More waiting……………….
These waiting times need some explanation. They were a very memorable time for all the family. Mentally, we were all gearing ourselves up for the worst news, and obviously this came with a bucket full of tears. With a few exceptions, we didn’t use to cry in the Green Room, we would take it in turns to go outside to what we later called “The Crying Bins”.
But, we used to laugh as well. Boy, did we laugh. Marie was chief food supplier for the hospital Pollard relatives. She used to bring in Quiche. She’d offer it round and Glenn (Marie’s husband) would decline it as would I.
Marie:- What is it with Quiche and men ?
Dp:- Quiche is more for homosexual men. Men eat Pies and Pasties, but not quiche.
So, of course, this became the running joke to any other male visitor who came, unaware of our in-joke, they would be offered Quiche, and if they said “Yes”, we’d all snigger.
Marie would also always have about 10 newspapers/magazines every day for everyone. She’d look for horses with Karen references in them and place a bet. I don’t think they ever won.
Another in-joke was the Handy Tips section of the women’s magazines. We would howl when these were read out. Things like…..
“Wrap your underwear and socks in your tights before putting them in the washing machine. That way, they’re all together when you empty it.”
“Don’t throw your old socks away, use them as gloves for dusting the house”
“If you’re getting your bathroom renewed, don’t throw your old toilet basin away, use it as a plant holder in the back yard”
Etc etc…
I hope that sets the flavour of “The Green Room” experience.
By 8pm on Day 2, I was getting anxious for news, so asked to see Frank for an update. Here’s how they recorded it…..
“David asked Frank what chances Karen had of surviving and was told at present 20-25% chance of survival maximum. Told them we are currently starting a medication to help with KP’s high pulmonary pressures and await effects.”
At the same time, they also recorded………
8pm – Becoming more acidosic … possible blood filtration tonight
By 9pm, she was on the Kidney Dialysis Machine.
Frank came to see us before going off for the weekend. He spoke to the family and as always I would push him for percentages of survival and along with an update said……
“I am back on Monday and I would be very surprised if Karen is still here then.”
![]()